When a man experiences inflammation of either one or both of his testicles, he is likely experiencing orchitis. Often, this is a problem associated with the same virus that is known to cause mumps. It is a common problem among males who have contracted the mumps, targeting a full third of them after puberty.
It is possible for other triggers to be responsible for causing orchitis, and it is possible for them to be bacterial, such as the presence of sexually transmitted diseases, or STDs. Some sexually transmitted diseases that may be to blame for orchitis include chlamydia or gonorrhea. More often than not, bacterial orchitis is the end result of the inflammation of the epididymis, which is the coiled tube, which is located behind the testicles and stores and transmits sperm. This is known as epididymitis, and when the orchitis is due to this, it is known as epididymo-orchitis.

Symptoms
The most common signs and symptoms of orchitis are swelling and pain. The symptoms for this condition usually are sudden to develop. Some of the symptoms might include:
- Testicular swelling, either on one or both sides
- Tenderness in either one or both testicles this may last for weeks
- Mild to severe pain
- Nausea
- Fever
- Discharge from the penis
- Blood in the ejaculate
- Not having been immunized against the mumps
- Being over the age of 45
Additional Symptoms Include
- Having had several urinary tract infections
- Having been born with a congenital abnormality within the urinary tract and
- Having had surgery that involved the urinary tract or the genitals, due to the risk of infection.
Things to Avoid:
- Several sexual partners
- Sexual encounters without a condom
- Sexual encounters with an infected partner or
Prepping for a Doctor’s Visit
- Write down every symptom that is being experienced, even if there does not appear to be any direct correlation between them and the orchitis.
- Write down any childhood illnesses and all vaccinations.
- Write down whether there have been any recent life changes or certain major stresses in life.
- List all medications, even supplements and vitamins, that are being taken.
- Take a family member to help soak in the information so that no piece of information is left missed or forgotten.
Questions to Ask Yourself
- What is likely the source of the pain?
- What are some other likely causes for this condition?
- What kind of tests will need to be performed?
- Is the orchitis likely to turn chronic?
- What is the best way to handle this?
- How can this be managed with other present conditions?
- Should a specialist be seen?
- Does the prescribed medicine have a generic alternative?
- Do not hesitate to ask any question that may arise throughout the duration of the appointment, such as clarifying certain points.
Questions a Doctor Might Ask
- When did the orchitis begin?
- How severe is the pain?
- What seems to improve the orchitis?
- What seems to worsen the orchitis?
- Any previous sexually transmitted diseases?
- Have the mumps ever been contracted or has there been a mumps vaccine? When?
- Is a condom always worn?
Sometimes, the terms “groin pain” and “testicle pain” are incorrectly interchanged with one another. However, the groin is located at the fold of skin between the abdomen and the thigh, and these are clearly not the testicles. Groin pain causes are different than that which are responsible for testicle pain.
When to See a Doctor
If there is any swelling or pain in the scrotum, especially if the development of the pain is very sudden, see the doctor for an appointment immediately.
There are several conditions that are known to cause pain in the testicles, and some of them do require immediate medical treatment. One example condition would be testicular torsion, in which the spermatic cord has been twisted, and this can cause a pain that feels similar to the one that is caused by orchitis. There are some tests that the doctor can conduct in order to figure out which specific condition is causing the pain in the testicles.
Causes
Orchitis may either be bacterial or viral.
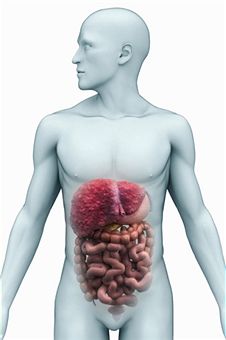
Bacterial Orchitis
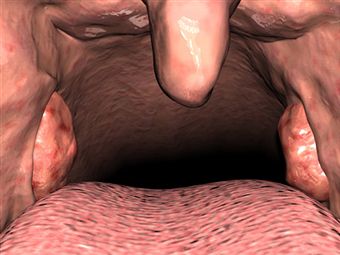
More often than not, when bacterial orchitis occurs, it occurs as a result of epididymitis, which is when the coiled tube connecting the testicle to the vas deferens becomes inflamed. The vas deferens is the part that is responsible for carrying the sperm from the testicles. When inflammation the inflammation present in the epididymis spreads all the way to the testicle, the condition that results from the occurrence is called epididymo-orchitis.
More often than not, a case of epididymitis is due to a man having an infection in his bladder or urethra, which ends up spreading out to the epididymis. The most common cause of this kind of infection is due to a sexually transmitted disease, or STD, and the specific disease is usually chlamydia or gonorrhea. There are other possible causes, include those that are in relation to having been born with some abnormalities of the urinary tract, or having had medical instruments or a catheter inserted into the penis.
Viral Orchitis
More often than not, viral orchitis is due to having had the mumps. One out of every three men who have ever had the mumps after puberty end up developing orchitis while they are still infected with the mumps, and this usually occurs within a week after it begins.
Risk Factors
There are several different factors that are thought to contribute to the development of non-sexually transmitted orchitis, such as:
When engaging in high risk sexual behavior, a man may get STDs that also increases the risk of developing sexually transmitted orchitis. Such behaviors include having:
Preparing for an Appointment with the Doctor
Most men will first start by visiting the general practitioner or a family doctor. However, sometimes, when calling up to make an appointment, he may find himself being referred immediately to another doctor whose specialties lie within urinary issues, or a urologist.
In order to get all of the information that is necessary from a doctor, it is helpful to be fully prepared for the appointment.
What Can Be Done
When calling to make the appointment, make sure to ask about whether or not there are any pre-appointment restrictions or if there is anything that might need to be done in advance, such as restricting parts of a diet.
Write down important questions to ask.
Time with the doctor is limited, and preparing questions ahead of time makes the process go quicker. In case time runs out, it is recommended to list the questions from most important to those that are not as important. With orchitis, some of the questions that might want to be asked include:
What to Expect from the Doctor
The doctor will probably have a list of questions to ask as well, so it is recommended to be prepared to answer them so that more time can be reserved for other parts of the appointment. Some questions that the doctor may ask may include:
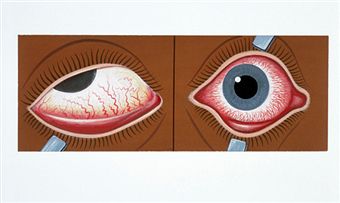
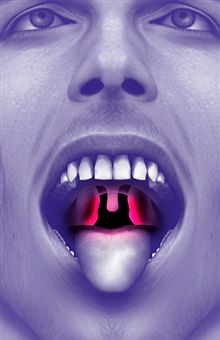
Tests and Diagnosis
The doctor will probably perform a physical examination to see whether or not there are any swollen lymph nodes in the groin or if the affected testicle is swollen. Both of these parts might be tender when touched. It is also possible that the doctor may wish to perform a rectal examination in order to check whether or not the prostate is enlarged or tender or to perform urine and blood tests to check for infection.
There may be other tests to determine if there is a sexually transmitted disease present and in order to tell whether testicular torsion has occurred, because this requires prompt and immediate treatment. Tests may include:
STD screening, which requires that the discharge from the urethra is obtained. To this, the doctor may need to insert a narrow swab into the head of the penis so that a sample may be obtained. The sample will be looked at beneath a microscope or it might be cultured to check for chlamydia or gonorrhea.
Urinalysis. Either collected at home during the morning or at the office, a sample of urine will be taken and sent off to a lab to see if any abnormalities exist in the concentration, appearance or content.
Ultrasound imaging. This makes use of high frequency sound waves that are able to create exact images of the structures found inside the body, and this is done in order to rule out the possibility of testicular torsion.
Treatments and Drugs
The necessary treatment for orchitis is dependent on what its cause is.
Treating Viral Orchitis
The actual treatment involved in handling viral orchitis, which is the kind that is related to the mumps, is to handle symptom relief. The doctor may prescribe pain medication or naproxen, as well as bed rest, which would require elevating the scrotum and also applying cold packs.
Treating Bacterial Orchitis
Aside from the steps required in order to relieve discomfort from the condition, treating epididymo-orchitis and bacterial orchitis will require antibiotics. The sexual partner will also require treatment if the cause is due to a sexually transmitted disease.
The antibiotics that are usually used in order to treat this kind of orchitis include doxycycline (Vibramycin, Doryx), azithromycin (Zithromax), ceftriaxone (Rocephin), trimethoprim and sulfamethoxazole combined (Bactrim, Septra), as well as ciprofloxacin (Cipro). Make sure the doctor knows what kind of medications are already being taken, in addition to any allergies. This information along with what kind of sexually transmitted disease is present and whether or not it is causing the orchitis will allow the doctor to find the best treatment option.
Ensure the infection is gone by taking the whole round of antibiotics as recommended, even if the symptoms should disappear before then.
Lifestyle, Home Remedies and Prevention
To relieve some discomfort try to lay in bed in a way that elevates the scrotum. If necessary, apply cold packs to the scrotum as well. Engage in safer sex, such as having a single sexual partner and using a condom this is very helpful towards protecting against sexually transmitted diseases.










 Depression is a mental health disorder that affects over 17 million Americans every year.
Depression is a mental health disorder that affects over 17 million Americans every year.