Body odor
Definition
Body odor is a very common problem that everybody has heard of or at least had the chance to smell! Most people understand that body odor and sweat are linked together but they do not know exactly how. According to dictionary.com, body odor is defined as an unpleasant odor from a perspiring or unclean person. There are many different names for body odor, including:
- B.O.
- Molodorousness
- Osmidrosis
- Bromhidrosis
- Ozochrotia
- Fetid sweat
Symptoms & Causes
Sweating and body odor are inexplicably linked to one another. Body odor is most likely to be caused by sweat, and sweating is a key reason for body odor. A few things that trigger sweating are exercise, a hot environment or hot weather, and nervousness. These are things that are very normal to most people and so they should be familiar with them.

Exercise involves exerting the body and causes the body to sweat in an effort to stay cool. The more the body undertakes strenuous activity, the more sweat that is produced.
If the weather outside is hot, those who have to be in the hot area will sweat. Exercise in a hot environment can produce even more sweat than normal.
Anxiety and nervousness are also major reasons for sweating, but cause sweating in specific places such as the face and the palms of the hands.
Sweat Effects
Sweat in and of itself has nearly no smell. It is very faint and can change depending on a person’s mood, diet, hormone levels, or drugs and medical treatments. What this leaves most people asking is this: If sweat is nearly odorless to human beings, why do sweating people always smell so bad?
The answer is that while sweat has no smell, as soon as it is released it comes into contact with bacteria on the skin. These bacteria begin to multiply quite rapidly in the presence of sweat and they cause the smell as well as explaining why it gets worse over time if not properly washed away.
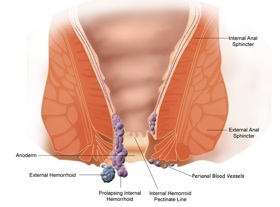
This is especially true of sweat that is the result of nervousness, anxiety, or stress. The body contains two types of sweat glands: eccrine glands and apocrine glands. Eccrine glands are the usual type and are distributed over the entire body. Apocrine glands tend to occur in places where hair grows such as the scalp, groin, and armpits. Eccrine glands secrete sweat when the body temperature rises and their job is to regulate body temperature.
Eccrine gland sweat is composed of water and salt for the most part and does not have an odor detectable to most humans. However, apocrine glands have no role in regulating temperature and instead control pheromones. They secrete a sweat that is fatty and gets pushed directly up onto the surface of the skin. Bacteria then begin to break it down, and the bacteria multiply. It is the breakdown of the bacteria that causes an odor, and this is what is most commonly referred to as body odor.
Risk Factors
Those most at risk for body odor are thus those who are more prone to sweating than others may be. Many studies show that the type of body odor a person has and how it is contrived is genetic. Major histocompatibility complex (MHC) molecules are what largely influence a person’s specific body odor, and they are 100% genetically determined.
How often a person sweats can also be largely influenced by the role of genetics. One study finds that East Asians sweat far less than most others, perhaps in adaptation to their colder climates. Though the studies show interesting results for different groups, one thing is clear for everybody: sweating is a genetic trait passed down and some people have the misfortune of inheriting genes which cause them to sweat heavily in noticeable areas such as the palms of the hands and soles of the feet.
It is also relevant to note that body odor is purely an adolescent and adult problem. Bromhidrosis (an alternative name for body odor) does not occur in humans until they hit puberty, so children do not ever have to worry about body odor.
This can cause confusion in teens who are experiencing puberty and do not realize that they are now at risk for body odor. Body odor is a very easily handled problem once these teens do realize that they must deal with it, but many cultures frown upon unpleasant body odor and so it may be quite embarrassing for them when they do realize this.
When to See A Doctor
Because the tendency of a person to sweat is a genetic trait, it is nearly impossible for doctors to define a “normal” sweating range to use for determining what is abnormal and medically problematic. For this reason, it is important for individuals to know what is normal for them.
Others may judge the amount one person sweats as irregular based on the amount that they sweat, but this would be an uneducated judgment. Instead, individuals should keep in mind what their normal amount of sweating and body odor is and use this to decide if there are any unusual changes or abnormalities occurring.
A change in the amount of sweating or in body odors may signal a problem, and so a doctor’s appointment should be made when this happens. Sweating more or less than the usual amount or randomly having night sweats are both causes for concern.
Body odor changing can be a sign of medical conditions such as diabetic ketoacidosis or kidney failure. Those who sweat excessively may also be interested in seeking medical attention for their problem, as sweating often and in large amounts can be extremely inconvenient and even embarrassing.
Preparing for the Appointment
An appointment can be made with the regular family physician or primary care doctor, or with a dermatologist. It is a good idea to call the primary physician first, as s/he will usually have a good idea of the individual background and might be able to pinpoint things that may be causing the abnormal sweating more easily than a dermatologist who does not have a personal history with a person.
Sometimes the primary physician will immediately refer skin questions to a dermatologist anyway, but it is still good to get a good recommendation from a trusted doctor, and the primary physician can provide this.
Playing the Waiting Game
Most doctors cannot see patients immediately and set up appointments, and once the appointment is set, it would seem that there is not much to do except wait. However, the staff at the Mayo Clinic came up with a list of a few things that people should consider doing while they are waiting for their appointment dates.
The first is to realize that appointments are often brief and time is limited, so a list of questions should be made to ensure that the patient does not forget any important questions that s/he feels need to be asked.
Remember that the doctor does not know everything about the problem the way that an individual does and can only take the information given to try and come up with a solution.
In order to help the process, the patient can write down the symptoms s/he is experiencing, when they first began, and any developments that occurred. Things that seem to worsen the symptoms or help them should be noted on the list as well as how frequently the symptoms occurred.
Tests & Diagnosis
Upon arrival at the doctor’s or dermatologist’s office for the appointment, the physician will usually conduct a physical exam and inquire about the patient’s medical history.

There are a few simple causes of a change in the amount of sweating or body odor. They are the presence of an overactive thyroid also known as hyperthyroidism or low blood sugar commonly referred to as hypoglycemia. Simple blood or urine tests can determine whether these are the cause of the symptoms and separate courses of action can be taken if they are.
Treatment & Dugs
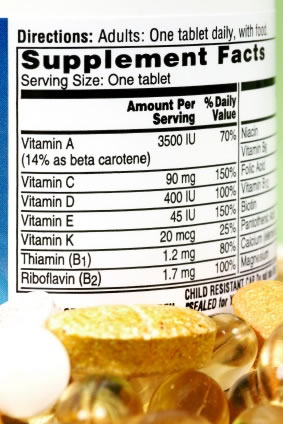
For most people, a doctor’s appointment will never be necessary in order to solve the problem of body odor. The very simple solutions of over the counter deodorants work for most. Deodorants do not do anything to stop the bacterial breakdown that is the cause of the body odor, nor do they stop the body from sweating.
They are alcohol-based products which help to control the odor by masking it with a more pleasant smell.
For a person whose average day does not involve much physical exertion or one who does not sweat often throughout the day, deodorants regularly applied to the underarms and possibly the hands and feet will be the only solution needed.
Though deodorants solve the problems of those with light sweating, many people exercise on a regular basis or just sweat more throughout the day, and deodorant is not enough to keep them from experiencing unpleasant body odor (and sharing it with everybody around them!).
For these people there are antiperspirants available that will help control body odor in a different way. Antiperspirants do exactly what they say; they help stop perspiration.
Aluminum Compounds
Most antiperspirants contain aluminum-based compounds that block the pores that secrete sweat for as long as the antiperspirant stays on the skin. In this way, less sweat reaches the skin and thus fewer odors is produced. Most antiperspirants contain a deodorant as well to help mask any odor that may still persist.
There are several special brands of deodorants and antiperspirants that strive to offer advanced protection against sweat and body odor. Secret and Gillette are two popular brand names that offer such products. As a personal aside, if you are looking for one such product that will help control body odor and sweating, I highly recommend that you should go online and see how actual users of the products have rated them. There are so many products available that it seems it would be quite difficult to choose one without research!
Most people put on a deodorant or antiperspirant at the beginning of each day and do not worry about the problem of body odor because this solves it effectively for them. For others, more is needed to help control sweating and body odor, and a doctor can suggest and prescribe these special treatments. The most commonly used is an aluminum chloride based antiperspirant such as Drysol or Xerac.
Usage of Antiperspirants
The antiperspirant is usually applied to sweat-prone areas before bedtime and then washed off completely in the morning to help control sweating throughout the day. A normal deodorant and antiperspirant combination usually costs no more than $5 for a stick that will last a few weeks or more.
Special aluminum chloride antiperspirants will cost $17-$25 comparatively and can be bought at drug stores and even Wal-Marts in some places, making them more costly but still relatively quite affordable and easily attainable for the average person.
Risks associated with treatment
Though the risks associated with most normal forms of treatment are small, they should not be ignored. Larger problems than excessive sweating or unpleasant body odor can arise from such ignorance. One very common problem with antiperspirants is that they do their job and block sweat, but nobody really thinks of where this sweat is going. Put simply, think of it this way: The body does not perspire to embarrass people or cause odors. Most of the time it does so because it needs to in order to regulate temperature and it is a natural occurrence.
Antiperspirants block sweat from coming through pores which stops sweat and body odor but can cause a number of other problems. The ingredients of antiperspirants can cause skin irritation which usually manifests itself as a slight burning or stinging that goes away. With the clinical-strength antiperspirants that are obtained from a doctor, this skin irritation tends to be much worse.
Skin Problems
The skin can become red, swollen, and itchy where the antiperspirant is applied. In addition to this, the sweat that was excreted from glands but not allowed to flow onto the skin because of antiperspirant-blocked pores can be trapped and cause cysts and infections. These are all very common problems associated with usage of antiperspirant products to control body odor and sweating.
Very few people have problems with deodorants and thus it is a safer solution, if less effective. Those who do experience skin irritation due to deodorants can usually solve their problems by selecting another deodorant that uses a different ingredient than the one that irritated their skin.
Alternative Treatments & Methods
Hyperhidrosis is the medical term that refers to excessive sweating. Excessive sweating is often the cause of excessive body odor because the two are inexplicably linked together; if the sweating can be solved, the body odor is then also solved. There are many herbal substances that are said to be effective in treating hyperhidrosis and the solutions to it range from these naturally-occurring herbal substances to botunlinum toxin (Botox) injections and surgery.
One such example of a natural herbal treatment is the administration of several herbs in tea form. There are various products available to those familiar with searching the Internet and purchasing products online. One such tea is called Hushed Tea and claims to be able to solve the problem of excessive perspiration through use of such herbs as valarian root, St. John’s wort, and sage. Sipping tea twice a day is much less invasive than botox injections or surgery and is also much more cost effective, and this may be a direction that many sufferers of hyperhidrosis can try for themselves.
Botox Injections
If natural remedies do not work, the next step on the ladder is botox injections. These are quite invasive and can be both painful and costly. Botox injections must be used in all of the places where excessive sweating occurs and the results do not last for very long, typically anywhere from four months to a year at maximum.
Several injections are usually required to obtain the desired results. Even with all of these downfalls, many people turn to botox injections to help deal with their hyperhidrosis because they are actually effective. The botox does not actually solve the problem though; it simply blocks the nerves that trigger the sweat glands and is a temporary fix.
Surgery Options for Body Odor
The final alternative for sufferers of hyperhidrosis is surgery to either remove the sweat glands causing the problems or interrupt the nerve signals to these sweat glands permanently. The Mayo Clinic is a well-known place to have the procedure done and its staff is very experienced with handling this type of surgery.
The success rates for surgery recipients are relatively high depending upon the problem area. For those with overly-sweaty palms, the chances of success are 95-98%. The armpits area has a 75-80% chance of success, and the feet show about a 25% chance of an improvement. Surgery of this type is never done solely to solve the problem of hyperhidrosis if only the feet are affected.
Those who undergo surgery to solve area-specific sweating problems will often notice more sweating on the torso area than they had before as a compensatory means to make up for the sweat that is not being excreted through the former problem area.
Most say that this is not a major problem for them as the compensatory sweat is not nearly as much as was excreted in the original problem area. The only other major difference is the realization that without sweat glands, areas such as the hands can actually become too dry and will need better care.
Prevention
In all reality, there is not much that anybody can do to prevent the fact that all people sweat. Some individuals may do so more than others. However, everybody does it. For most, sweating and body odor are very small problems if they are problems at all and they can be easily solved using the techniques listed above.
For a smaller percentage of people, hyperhidrosis is a problem that causes much stress and anxiety as well as accompanying body odors that can have a substantial effect on the lives of the sufferers. Sweating is a natural occurrence that causes body odor for most and bigger problems for some.